A practical understanding for parents and providers
Written By
Kyle McEvoy, MS LMHC, LPC, NCC, CCMHC
Tags: Self-Harm, Support, Emotion, Coping, Skills
Adolescence is a challenging period characterized by physical, emotional, and psychological changes. For some adolescents, navigating this transitional phase can be particularly difficult, leading to behaviors that are harmful to themselves, notably self-harm. Self-harming behaviors among adolescents have become a growing concern in recent years, prompting the need for a deeper understanding of its fundamental elements. In this blog, we delve into the roots and dynamics of adolescent self-harming behaviors, exploring the underlying causes, risk factors, and potential interventions.
Self-harm, also known as self-injury or self-mutilation, refers to the deliberate act of inflicting harm on one’s own body without the intent to die. It is often a coping mechanism used by individuals to manage overwhelming emotions or to communicate distress when they lack the necessary coping skills. Self-harm can take various forms, including cutting, burning, scratching, hitting, or excessive substance abuse.
Understanding the Motivation Behind Self-Harm:
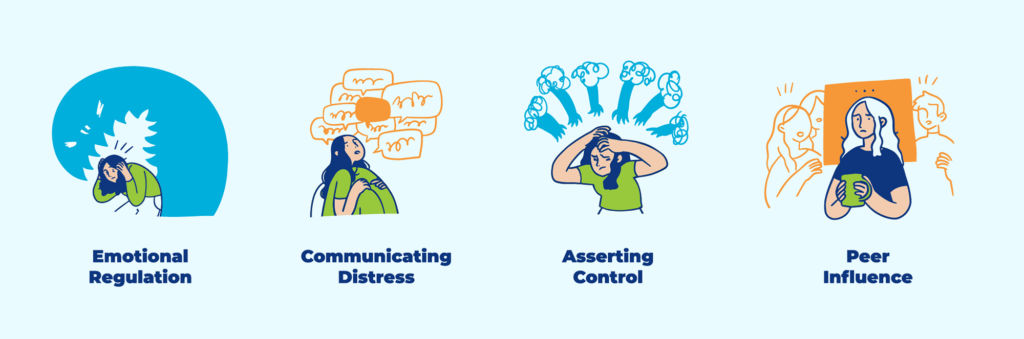
- Emotional Regulation:
- Adolescents may resort to self-harm to regulate overwhelming emotions such as anger, sadness, or anxiety. The physical pain inflicted during self-harm can temporarily distract from emotional pain, providing a sense of relief.
- Communication of Distress:
- In some cases, self-harm is a way for adolescents to communicate their internal struggles and distress when they feel unable to articulate their emotions verbally. Feelings of guilt, shame, or self-loathing can drive adolescents to self-harm as a form of punishment for perceived inadequacies or mistakes.
- Control and Autonomy:
- Adolescents may engage in self-harm to exert control over their bodies and experiences, especially in situations where they feel powerless or marginalized.
- Peer Influence:
- Peer pressure and social dynamics can also play a role in the initiation and perpetuation of self-harming behaviors among adolescents, particularly in group settings.
Risk Factors Associated with Adolescent Self-Harm:
- Mental Health Disorders:
- Adolescents struggling with mental health issues such as depression, anxiety, borderline personality disorder, or post-traumatic stress disorder (PTSD) are at a higher risk of engaging in self-harming behaviors.
- History of Trauma:
- Exposure to traumatic events, including physical, emotional, or sexual abuse, neglect, or witnessing violence, can significantly increase the vulnerability of adolescents to self-harm.
- Family Dynamics:
- Dysfunctional family environments characterized by conflict, instability, neglect, or parental substance abuse may contribute to the development of self-harming behaviors in adolescents.
- Peer Pressure:
- Peer relationships and social dynamics, including bullying, rejection, or a lack of supportive friendships, can influence adolescents to engage in self-harm as a coping mechanism or as a means of fitting in with peer groups.
- Low Self-Esteem:
- Adolescents with low self-esteem or negative body image may turn to self-harm to cope with feelings of inadequacy or to seek validation from others.
- Academic Pressure:
- Academic stress, performance anxiety, and unrealistic expectations imposed by parents or educators can contribute to the emotional distress experienced by adolescents, potentially leading to self-harming behaviors.
Intervention strategies:

Addressing adolescent self-harming behaviors requires a multifaceted approach that addresses underlying emotional needs while providing support and resources for recovery:
- Psychotherapy:
- Cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), Mentalization based treatment (MBT) and other evidence-based therapeutic modalities can help adolescents develop healthier coping mechanisms, regulate emotions, and address underlying issues contributing to self-harm.
- Family Therapy:
- Involving family members in the therapeutic process can foster better communication, improve family dynamics, and provide a supportive environment for adolescents to address underlying issues contributing to self-harm.
- Peer Support Groups:
- Peer-led support groups or group therapy sessions can offer adolescents a sense of belonging, validation, and peer support from individuals who have experienced similar challenges.
- Psychiatric Evaluation and Medication:
- In cases where underlying mental health disorders contribute to self-harming behaviors, psychiatric evaluation and medication management may be necessary as part of a comprehensive treatment plan.
- School-Based Interventions:
- Schools can implement prevention programs, mental health education initiatives, and counseling services to support adolescents and create a supportive environment that promotes emotional well-being.
- Community Resources:
- Collaborating with community organizations, mental health professionals, and support networks can expand access to resources and provide ongoing support for adolescents and their families.
How to Be Supportive:
Supporting someone who is engaging in self-harm can be challenging, but it is essential to offer compassion, understanding, and appropriate assistance. Here are some ways to support someone who is self-harming:
- Listen without judgment:
- Create a safe and non-judgmental space for the individual to express their feelings and experiences. Avoid reacting with shock or anger, as this may deter them from seeking further support.
- Validate their feelings:
- Acknowledge the individual’s emotional pain and validate their experiences without minimizing or dismissing them. Let them know their feelings are valid and you are there to support them.
- Encourage open communication:
- Encourage the individual to talk about their thoughts and feelings, including the triggers and underlying reasons for their self-harming behaviors. Be patient and empathetic, as they may find it challenging to articulate their emotions.
- Express concern and care:
- Express your genuine concern for the individual’s well-being and let them know that you care about their safety. Reassure them that they are not alone, and that help is available.
Additional Supports:
- Offer practical support:
- Help the individual explore alternative coping mechanisms and strategies for managing their emotions in healthier ways. This may include suggesting activities they enjoy, practicing relaxation techniques, or seeking professional help.
- Provide resources:
- Offer information about available resources and support services, such as hotlines, counseling, therapy, or support groups. Assist them in accessing these resources if needed.
- Respect their boundaries:
- Respect the individual’s autonomy and boundaries and avoid pressuring them to stop self-harming before they are ready. Let them know that you support them whenever they are ready to seek help.
- Educate yourself:
- Take the time to educate yourself about self-harm, its causes, and available treatments. Understanding the nature of self-harm can help you provide more effective support and guidance.
- Involve trusted adults:
- If the individual is a minor, involve trusted adults such as parents, guardians, teachers, or mental health professionals to ensure they receive appropriate support and intervention.
- Practice self-care:
- Supporting someone who is engaging in self-harm can be emotionally taxing. Remember to prioritize your well-being and seek support from friends, family, or mental health professionals if needed.
Encourage professional support:
It is important to remember that supporting someone who is self-harming may require ongoing patience, understanding, and persistence. Encourage the individual to seek professional help from a therapist, counselor, or psychiatrist who can provide specialized support and treatment tailored to their needs.
Adolescent self-harming behaviors are complex phenomena influenced by many factors, including emotional distress, social dynamics, and underlying mental health issues. By understanding the fundamental elements of self-harm and addressing its underlying causes, we can better support adolescents in navigating their emotional challenges and fostering healthier coping mechanisms. Through therapeutic interventions, family support, peer networks, and community resources, we can empower adolescents to heal and thrive during this critical stage of development.
References:
American Psychological Association. (2022). Understanding self-harm. Retrieved from https://www.apa.org/topics/self-harm.
Hawton, K., Saunders, K. E., & O’Connor, R. C. (2012). Self-harm and suicide in adolescents. The Lancet, 379(9834), 2373-2382.
Klonsky, E. D. (2011). Non-suicidal self-injury in United States adults: Prevalence, sociodemographics, topography and functions. Psychological Medicine, 41(9), 1981-1986.
Madge, N., Hawton, K., McMahon, E. M., Corcoran, P., De Leo, D., de Wilde, E. J., … & Arensman, E. (2011). Psychological characteristics, stressful life events and deliberate self-harm: Findings from the Child & Adolescent Self-harm in Europe (CASE) Study. European Child & Adolescent Psychiatry, 20(10), 499-508.
Muehlenkamp, J. J., & Gutierrez, P. M. (2007). Risk for suicide attempts among adolescents who engage in non-suicidal self-injury. Archives of Suicide Research, 11(1), 69-82.
National Alliance on Mental Illness. (2022). Self-harm. Retrieved from https://www.nami.org/About-Mental-Illness/Common-with-Mental-Illness/Self-harm.
National Institute of Mental Health. (2022). Self-harm. Retrieved from https://www.nimh.nih.gov/health/topics/self-harm.
Nock, M. K. (2009). Why do people hurt themselves? New insights into the nature and functions of self-injury. Current Directions in Psychological Science, 18(2), 78-83.
Nock, M. K., & Prinstein, M. J. (2004). A functional approach to the assessment of self-mutilative behavior. Journal of Consulting and Clinical Psychology, 72(5), 885-890.
Royal College of Psychiatrists. (2022). Self-harm. Retrieved from https://www.rcpsych.ac.uk/mental-health/problems-disorders/self-harm.
Whitlock, J., Knox, K. L., & Eckenrode, J. (2006). The relationship between self-injurious behavior and suicide in a young adult population. Archives of Pediatrics & Adolescent Medicine, 160(2), 150-156.
Whitlock, J., Muehlenkamp, J., Eckenrode, J., Purington, A., Baral Abrams, G., Barreira, P., … & Knox, K. (2013). Nonsuicidal self-injury as a gateway to suicide in young adults. Journal of Adolescent Health, 52(4), 486-492.
Zetterqvist, M. (2015). The DSM-5 diagnosis of nonsuicidal self-injury disorder: A review of the empirical literature. Child and Adolescent Psychiatry and Mental Health, 9(1), 31.


You must be logged in to post a comment.